In October 2004 the American Association of Colleges of Nursing (AACN) membership voted to require the Doctor of Nursing Practice (DNP) as the entry level degree for all new advanced practice nurses by 2015. At the time of the October 2004 vote there was only one DNP Program in the country, but the AACN proceeded to align itself with this one degree model. Was this vote for the 2015 mandate hasty or perhaps bold? Was the DNP model so singly endorsed, embraced prematurely? This article discusses the broader context of why the DNP should not be the only practice doctorate degree model offered and why the clinical research Doctor of Nursing Practice (DrNP) degree at Drexel University should be a viable alternative. In development since 2000, the Drexel Model DrNP is a hybrid degree combining the professional practice doctorate and the academic research doctorate. Unlike the DNP, it includes a clinical dissertation that will prepare a ‘practitioner/researcher’ to help advance the evidence base of nursing.
Key Words: DrNP, practice doctorate, clinical research doctorate, DNP, Drexel DrNP
The American Association of Colleges of Nursing’s adoption of the Doctor of Nursing Practice (DNP) as the entry level practice degree for advanced practice nurses by 2015 looms like a turbulent maelstrom (AACN, 2004a). It became clear at the January 2005 AACN Doctoral Education Conference that the political issues associated with this degree are real and need to be more fully addressed. In the limited time made available for public discussion of the DNP at that conference, the following issues emerged:
- Some members of the National Organization of Nurse Practitioner Faculties (NONPF) fear that the initials "DNP" will lead the public to assume that all clinicians with those letters after their names are nurse practitioners (O’Sullivan, 2005). They would prefer to have the practice doctorate be indicated by the letters "DPN" (Doctor of Practice of Nursing). Independent of NONPF, the Executive Director of the American College of Nurse Practitioners reports they do not yet have an official position on the DNP (C. Hutcherson, personal communication, November 16, 2005). Last, the largest NP organization, the American Academy of Nurse Practitioners, has just published a discussion paper which appears to somewhat support the DNP, but which raises eight major concerns (2005).
- Some nurse midwives have been quietly talking about a Doctor of Midwifery (DM) (Stein-Parbury, 2000) and indicate they have not been fully consulted about this proposal. Further, in June 2005 the American College of Nurse Midwives (ACNM) Division of Accreditation Governing Board affirmed that the Doctor of Nursing Practice may be one option for some nurse-midwifery programs, but that the ACNM "does not support the DNP as a requirement for midwifery education" (p. 1).
- Clinical nurse specialists feel perhaps marginalized by several forces: the primary care focus and NONPF forces behind the practice-doctorate and the Clinical Nurse Leader (CNL) movement. In the past year the National Association of Clinical Nurse Specialists (NACNS) has issued detailed white papers indicating their opposition to both the DNP (2005a) and the CNL (2005b). In response to this the AACN is now circulating a draft document which outlines their support for the CNS role (AACN, 2005a).
- It is also not clear whether nurse anesthetists are seriously considering entry level doctoral preparation or the "DNP" model either (Kinslow, 2005). In 2003 the Council on Accreditation of Nurse Anesthesia Programs mandated that all Program Administrators of Nurse Anesthesia Programs have the doctorate by 2014. However, in January 2004, less than one year later, they retracted this mandate in favor of language saying the doctorate would be "preferred" (p. 2). While this organization continues to study this issue, they recently indicated they do not support the 2015 target date (AANA, 2005).
- The DNP model has not been universally endorsed by colleges and universities with graduate nursing education programs for a variety of reasons. Reasons range from a fear of the consequences of this model for existing master’s and PhD programs to a realization that a move to require the entry level practice doctorate is likely to result in the closure of masters nursing programs in colleges without doctoral charters. Realistically, how many college faculties are going to vote to amend their charters to permit nursing to offer their first doctoral degree, especially a professional doctorate?
Before we move to standardize curricula and accredit DNP programs, we should explore what we might gain from diverse approaches in doctoral nursing education. - Even among universities prepared to offer a doctor of nursing practice degree, the proposed DNP model has not been fully embraced. Both Columbia University and Drexel University have chosen to initiate DrNP degrees instead. Even the National Academy of Sciences, somewhat contrary to the strong endorsement reported recently on the AACN website (2005b), indicates "the concept of a nonresearch clinical doctorate in nursing is controversial" (2005, p. 7).
This paper will offer a critique of the DNP degree and then describe the Drexel DrNP Model and why it should be a credible and viable alternative practice doctorate. The underlying assumption of this paper is that nursing education can benefit from more experimentation, innovation, and creativity, not less. Before we move to standardize curricula and accredit DNP programs, we should explore what we might gain from diverse approaches in doctoral nursing education.
Should the DNP Be the Only Viable Practice Doctorate Model?
...is there real substantive consensus to boldly say the DNP model is the only appropriate practice-doctorate model for all advanced practice nurses? |
We pose the following question: do we know enough yet and is there real substantive consensus to boldly say the DNP model is the only appropriate practice-doctorate model for all advanced practice nurses? Some panelists and participants at the 2005 AACN Doctoral Education Conference observed that many PhD students never conduct any research beyond their dissertation and concluded that the DNP degree would have been the more appropriate alternate doctorate for them. We disagree. Our four focus groups with advanced practice nurses (APNs) conducted on-site at local hospitals in Philadelphia confirmed that many prospective doctoral nursing students first do not fully understand the differences between the professional and the academic doctorate. More critically, they also generally do not entirely understand the implications that completing either type of doctoral degree has for their future career options. This leads us to four central issues involved in promoting the DNP as the only standard practice doctorate model.
First we emphasize that many professional (or practice) doctorate programs are actually hybrids of both the professional-practice and academic-research doctorate degree. Examples include the Doctor of Public Health (DrPH), Doctor of Psychology (PsyD), Doctor of Social Work (DSW), the Doctor of Science in Audiology (ScD) at Boston University (2004), or the Doctor of Science in Physical Therapy (DScPT) at University of Alabama at Birmingham (2005). Most often these programs do require the student to conduct a research study and not merely a research utilization project. Our point is that there is precedent for creating a hybrid professional doctorate degree with a clinical dissertation requirement. Further, the model of the professional doctorate as a completely non-dissertation (research) doctorate is not a global one. At the University of Queensland in Australia, ‘professional doctorates’ are defined as "coursework programs which allow experienced professionals to return to study to improve their professional practice through the application of research to current problems and issues. This qualification combines coursework and research, with a component of not less than 33% and not more than 66% research. The doctoral research should make a significant contribution to the knowledge and practice of the profession" (2004, p.1).
What we need is a group of trained clinical researchers who will be adept at identifying from their clinical practice critical problems that can be investigated in the clinical context. |
The second issue relates to the premise that since many nursing PhD graduates are not engaged in research beyond their dissertations, putting students into DNP rather than PhD programs should have little net effect on the state of nursing scholarship. This premise, however, ignores the potential drain on faculty and budgetary resources that will result from widespread initiation of DNP programs. PhD graduates who might have moved into faculty positions in research-intensive universities where they could be mentored as nurse scientists are likely to be siphoned off (perhaps even lured by lucrative salaries) to fill teaching-intensive faculty positions in DNP programs, reducing even further the numbers of PhD trained, active researchers. We therefore foresee a possible trend toward an overall decrease in nursing faculty members engaged in knowledge development with the proliferation of DNP programs, something the discipline of nursing does not need or cannot risk. We also pose the following hypothetical question – if every APN in 2015 were to obtain a DNP, we wonder exactly who is left to pursue the PhD? What we need instead is a group of trained clinical researchers who will be adept at identifying from their clinical practice critical problems that can be investigated in the clinical context. We predict Magnet facilities in particular will be very interested in hiring these kinds of practitioner/researcher APN graduates.
Issue three: there is a risk that DNP graduates who wind up in academia will be marginalized. We predict it is possible the DNP degree may unintentionally disenfranchise a future generation of highly educated nurses, a feeling similarly echoed by Gennaro (2004) and the NACNS (2005a). The new ‘DNP’ is much more like the Doctor of Physical Therapy (DPT), Doctor of Pharmacy (PharmD), or Doctor of Occupational Therapy (OTD) degrees that do not require the dissertation. Therefore, these graduates are not educated for faculty positions; yet they might ultimately pursue an academic career. Assume that after two years a DNP graduate wants to leave practice and become a nursing professor and teach full time. Is this individual qualified for a tenure-track faculty position? The unavoidable answer is that the DNP graduate, with no research dissertation, will not be hired for tenure-track positions by most universities. And what will happen if the DNP graduate is hired at a small college and sits down at a table with a PhD Sociologist who says, "So what was the topic of your nursing dissertation?" And she gulps or winces and replies, "I didn’t do one." Once again, nursing will be in the awkward position of sitting at the academy table with ‘less-than’ credentials. This would be an enormous set-back for nursing academia which still only has 49.7% of its nursing professors (in baccalaureate or higher nursing education) currently prepared at the doctoral level (AACN, 2004b).
...there is a risk that DNP graduates who wind up in academia will be marginalized. |
Finally, issue four pertains to a widespread misconception that health professionals are educationally prepared through a single, designated degree program, e.g., all physicians are awarded the MD. In fact, multiple degree models are common for health professions occupations. For example, both medical doctors (MD) and osteopaths (DO) operate within the same domain of practice through different educational preparations and degrees. According to the American Dental Association (ADA), dentists with either the Doctor of Dental Medicine (DMD) or the Doctor of Dental Surgery (DDS) have the same education. "Universities have the prerogative to determine what degree is awarded. Yet both degrees use the same curriculum requirements set by the ADA’s Commission on Dental Accreditation" (2005, p. 1). Even veterinarians have the DVM and VMD (both a Doctor of Veterinary Medicine)! Lest we think we still should only have the DNP, we believe the argument that ‘the public will be confused!’ is therefore very weak indeed.
The Evolution of the Drexel Model DrNP
The Drexel DrNP is not the same as the DNP degree, which the AACN has proposed as an entirely non-research doctorate. It is, nonetheless, a doctor of nursing practice degree that includes two doctoral practica and a curriculum built around a nursing science and nursing practice core. When the Drexel University School of Public Health made the decision in 2003 to offer the DrPH rather than the PhD, Drexel’s nursing faculty began to more seriously ask whether an equivalent research-based practice doctorate might be appropriate in nursing. The DrPH degree has a long established history in the United States and is an academic, research doctorate more focused on public health practice than the traditional PhD in Public Health. More than 25% of DrPH programs nationally have a field practicum requirement (Lee, Furner, Yager, & Hoffman, 2003). Since the Drexel Doctoral Nursing Program Development Committee had envisioned a "practitioner/researcher" model of doctoral nursing education since 2000, the nursing faculty saw an opportunity to develop a parallel degree (DrPH vs. DrNP). Like the DrPH, the Drexel DrNP is a practice-focused, academic doctorate requiring the completion of a clinical dissertation that will generate evidence-based nursing science. The developers of Drexel’s clinical research DrNP in Nursing Science see their hybrid degree, part professional-practice and part academic-research doctorate, representative of what Christensen and Raynor (The Innovator’s Solution, 2003) would call ‘disruptive innovation.’
From the outset, Drexel’s faculty was aware of the first DNP model at the University of Kentucky, but chose not to emulate it for a number of reasons. Chief among these was a concern to address the severe nursing faculty shortage, which the DNP degree by explicit design does not do. The Kentucky DNP offers a curriculum with a Clinical Leadership or Executive Management track, but it does not prepare APNs or nurse educators. While the PhD is and will continue to be the degree most appropriate for those seeking careers in research-intensive universities, nursing also has a need for clinical faculty members who can engage in evidence-based nursing practice themselves while imparting their expertise to students (Fitzpatrick, 2003). The clinical research DrNP will provide nursing faculty members with a credible hybrid doctorate, giving them both practice skills and the research experience necessary to underpin the professorial role and thus the concomitant credentials recognizable in academia. This, however, does not mean that the DrNP is a substitute for the PhD. It is a practice-doctorate with a clinical research focus. Nurses holding the DrNP will not generally be expected to independently conduct large scale empirical research. Rather, they will be capable of conducting clinical research in practice settings, of participating on and even leading as members of interdisciplinary research teams, and of engaging in evidence-based, informed nursing practice in a variety of settings.
If this degree is not a DNP, nor PhD, is this degree really a DNSc, DNS, or DSN? We portend it is not. In reality, the DNSc, DSN and DNS have largely become de facto PhD degrees and regarded as such. It is unfortunate that university politics (sometimes elitist prejudice by other scientific disciplines against nursing science) have generally prevented the proper conversion of many of these programs to the PhD. The University of Alabama at Birmingham is a good example of a DSN program that converted to the PhD in 1999. However, our review of the eleven remaining DNSc, DNS or DSN programs in the US indicates there is no consistent inclusion of clinical nursing practica in them and the majority do not have any. Nevertheless, we think the historic evolution of these programs now prevents their practical re-engineering away from the PhD model. Thus we view our clinical research Doctor of Nursing Practice (DrNP) in Nursing Science as a doctorate of ‘the practice of nursing science,’ and therefore our curriculum is structured equally around a nursing practice and nursing science core. We suggest that as these other degree models have served their purpose historically, it is time the remaining DNSc, DSN, and DNS programs convert to PhD in Nursing Science programs especially if they have the resources or Carnegie Classification to compete for NIH funding. If the aim is not to be a de facto PhD, then they should consider truly distinguishing themselves from the PhD by becoming clinical research doctor of nursing practice in nursing science programs, not doctor of nursing science programs in their various iterations.
Finally, we note that our DrNP in Nursing Science is different from the DrNP model at Columbia University. At the 2005 AACN Doctoral Education Conference Columbia advertised their program as a ‘DrNP in Primary Care,’ but their current website describes their program as a ‘Clinical Doctorate.’ We actually liked their original DrNP in Primary Care model to prepare nurse practitioners, but only regret they have not included a clinical dissertation. We suggest, whether fair or not, that if doctorally-prepared NPs (or APNs) truly want parity or equity with physicians, then their education preparation needs something that would give them ‘extra value’ over the MD. We contend this ‘extra value’ is clinical research skills that physicians only learn through the apprentice model.
The Drexel Model DrNP in Nursing Science: The Clinical Research Doctorate of Nursing Practice Curriculum
...our focus groups included a surprising number of nurse managers and executives who were also seeking a practice-focused nursing doctorate. |
The Drexel DrNP in Nursing Science is designed as a generalist practice doctorate (versus a DrNP in Primary Care) for the Master’s prepared Registered Nurse who seeks a doctoral degree that focuses on nursing practice and clinical nursing research (see Figure). In 2004 we surveyed 168 APNs about our model (Dreher et al., 2005) and the results confirmed several of our suppositions. First, the majority of focus group participants did not see full-time PhD study as a realistic option and were enthusiastic about a cohort model where the degree could be completed in three years. Participants also endorsed the clinical research practice doctorate model and we did not discern any measurable resistance to clinical research or the desire for a doctorate with no dissertation. On the contrary, many of the APNs had actively participated in clinical trials and wanted more practical research skills. This confirmed our creation of a secondary Clinical Scientist Track. Similarly, our focus groups included a surprising number of nurse managers and executives who were also seeking a practice-focused nursing doctorate. This likewise confirmed our offering of a secondary Clinical Executive Track. Finally, focus group participants requested we decrease our required doctoral practicum hours, as our original proposal was perceived as too burdensome for them to complete and simultaneously maintain full-time employment.
Based on this data, we project that 45% of our matriculants will select the Practitioner Track, 36% will select the Educator Track, 12% the Clinical Executive Track, and 7% the Clinical Scientist Track. We also anticipate a significant number of our Practitioner Track graduates will eventually enter nursing academia or perhaps pursue joint faculty/clinical appointments within their institutions after several years. The DrNP admissions process is not geared to admitting a certain number of students in each track, but rather to matching each student's clinical and research interest to those of the Graduate Research Faculty. Our degree has the following primary curricular objectives:
- Establish a theoretical nursing science background for analyzing clinical nursing phenomena
- Build upon the clinical practice knowledge of each student
- Enhance each student’s knowledge base with a specialized clinical practicum of their choosing
- With a specialized role practicum, support the importance of role development for clinical nursing scholars with the doctorate who may choose from a variety of career opportunities
- Emphasize clinical nursing research with the aim of improving health across the lifespan through scientific inquiry
Figure. The DrNP in Nursing Science
The curriculum is constructed around five core fields: 1) Nursing Science Core; 2) Nursing Practice Core; 3) Research Methods Core; 4) Cognate Core; 5) Dissertation Core
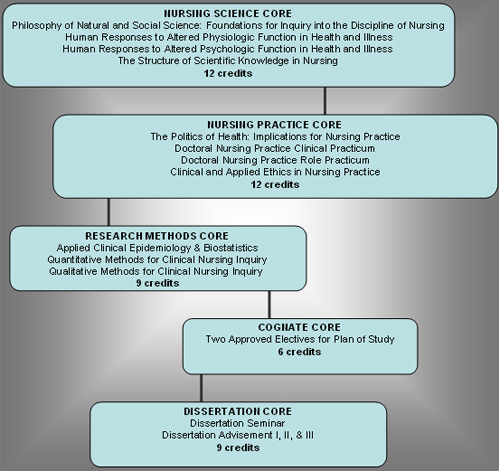
Residency Requirement: Must complete both Summer Residency Weeks
Total Credits: 48 Quarter Credits Minimum
This DrNP program is designed for the doctoral student who seeks one of four different career tracks:
The Practitioner Track: The Clinical Scholar in Advanced Nursing Practice - a Primary DrNP Focus
One primary track is designed for practicing nurses who want to obtain a nursing doctorate for career advancement, but who also want to engage in clinical scholarship and research that can be integrated with their full-time advanced nursing practice positions. One example of a typical candidate might be a midwife who chooses to do a Clinical Practicum in infertility to gain more in-depth expertise in this area. This same student might also see her midwifery practice as increasingly requiring more technology-supported administrative skills. Therefore, this student selects an administrative Role Practicum to explore ‘best-practice’ clinical technology support systems to help her optimize the administrative and managerial functions of running a midwifery practice.
The Educator Track: The Clinical Scholar in Nursing Education – a Primary DrNP Focus
The DrNP is also primarily designed for practicing nurses who want a clinical nursing doctorate and to continue or begin roles as nursing faculty members. A typical candidate might be a Master’s prepared Family Nurse Practitioner who has been doing some part-time preceptor teaching in a local FNP program. He chooses a cardiac rehabilitation Clinical Practicum, for example, and then selects a teaching Role Practicum to be better prepared for a full-time teaching position upon graduation. It should be noted that because this is a doctor of nursing practice degree designed to develop clinical scholars, Educator Track students cannot conduct a nursing education-oriented dissertation unless it has a clear clinical practice focus.
The Clinical Executive Track: The Clinical Scholar in Nursing Leadership & Healthcare Management - a Secondary DrNP Focus
While the DrNP is primarily designed to prepare practitioners and educators, this degree may still be appropriate for the nurse manager or executive who desires a doctoral program with a connection to clinical practice. An individual in this track could do any type of Clinical Practicum and the Role Practicum could concentrate on executive areas identified by the student as needing more development. The student could use the cognates to take courses in health economics or finance. The clinical dissertation topic, however, would focus on some aspect of clinical nursing management such as a cost-effectiveness clinical intervention analysis.
The Clinical Scientist Track: The Clinical Scholar in Nursing & Health Research - a Secondary DrNP Focus
Finally, a secondary track is available for individuals whose goal is to gain beginning skills as clinical scientists. A typical student could be an Oncology Clinical Nurse Specialist who wants to gain the research skills to serve as a Primary Investigator (PI) on oncology-focused clinical trials at her teaching hospital and Magnet institution. Having a DNP degree without the experience of dissertation research would not give this APN the necessary research skills to credibly lead a clinical research team. However, the CNS pursuing the Drexel DrNP degree would have these skills. She could do her Clinical Practicum by working in a cancer genetics clinic, for example, and then complete a research Role Practicum focusing on clinical trials management with an experienced clinical trials/scientist mentor.
Curricular Logistics of the Clinical Research DrNP Degree
The logistics of our curriculum and course scheduling were particularly constructed for the working APN. We schedule all classes one day a week (from 2:30 pm to 8:30 pm), and utilize a cohort model, requiring year-round attendance (albeit part-time) in a three-year curriculum, quarter-credit format. Students take two courses each Fall, Winter, and Spring quarter and one course in the summer for two years. The third year is exclusively geared to the conduct and completion of the clinical dissertation. Students also attend a week long summer residency at the end of the first and second year with a Clinical-Scholar-in-Residence and where DrNP students take part in activities designed to socialize and help develop the clinical scholar. These activities include a doctoral scholarship symposia where first and second year students will present their best written papers over the previous year in oral format (open to all students and faculty in the College) and receive evaluation of their performance; participate in a qualitative software workshop and a PDA update workshop; receive instruction in professional curriculum vitae construction; attend a panel discussion on career counseling from nurses who are already experienced practitioners, educators, clinical executives, and clinical scientists; and many other activities. The specific track selected by each student guides the advisement process, the cognate selection, the objectives and sites for the two doctoral nursing practica, and career counseling. The Table below describes the primary didactic content covered in each of the two doctoral practica which are 40-60 hours minimum in length. The clinical practicum is designed to extend the student’s clinical knowledge base in some additive way. The role practicum focuses more on role delineation and related skill acquisition for the individual student (i.e., test item analysis skills perhaps for the Educator Track student or conflict resolution and negotiation skills for those in the Clinical Executive Track).
Table. Didactic Content Covered in Doctoral Nursing Practica
|
NURS 830: Doctoral Nursing Practice |
NURS 835: Doctoral Nursing Practice |
|
Models of the reflective practitioner (i.e., how developing a reflective approach to clinical care can enhance both therapeutic potential and health outcomes) |
Role negotiation theory (i.e., how to challenge pay equity issues in the doctorally educated nursing workforce, especially for women) |
|
Interdisciplinary novice-to-expert theories |
Seeking lifelong mentorship and menteeship |
|
Use of evidence-based data bases to drive interventions |
Analyzing one’s leadership abilities and developing a professional development trajectory |
|
Cost effectiveness evaluation of clinical interventions |
Stress management and role strain for the doctorally educated nurse |
The Clinical Dissertation for the Drexel DrNP: The PsyD Model
The clinical dissertation for the DrNP degree will be modeled after the clinical dissertation that has been widely successful and implemented by most Psychology Doctorate (PsyD) programs (Rutgers University, 2005; Wheaton College, 2004; Widener University, 2005). The PsyD degree was developed in the late 1960s (after heated debate) to prepare a hybrid scientist-practitioner. It came into existence because the PhD in Clinical Psychology was increasingly focusing on experimental research and preparing students primarily for research careers, and thus a growing demand for a more practice-oriented clinical psychology degree evolved (Peterson, 1976; 1982). Donald Peterson, a pioneer in the PsyD movement has described PsyD graduates as being trained as "local scientists" who apply the scientific method to problems in the field (Murray, 2000, p.1). The PsyD 'clinical dissertation' has a distinct clinical practice orientation and is designed to be completed typically in one year, but differs in both scope and in its applied emphasis from the traditional PhD dissertation. Sample dissertation topics from Rutgers University’s PsyD program can be viewed at their website. We contend a more highly supervised and more structured dissertation process (especially for a practice discipline) can decrease the inordinate amount of time spent writing the proposal, getting through IRB, collecting and analyzing data, and then finally writing (and revising) the final document. For example, several of our faculty spent 1-2 years just collecting data.
In setting our own structured procedures for completion of the clinical dissertation, we used a dissertation consultant from the oldest PsyD program in the country. Our structured process begins when students select a clinical nursing research question by the third quarter of study. This selection follows the completion of three nursing science courses in the first year that examine common physiological and psychological clinical variables (i.e., sleep, pain, stress, coping, self-efficacy, and others). The question must then be approved by a committee that ensures the proposed clinical research question is both germane to nursing practice and within the scope of this degree. Subsequently, students will be required to write the first draft of their dissertation proposal in their quantitative or qualitative methods courses (not both) in the 4th or 5th quarter of study with a research design that will generally permit data collection over a 3-4 month period. Additionally, the qualifying exam taken at the beginning of the second year must focus on a variable or concept in the student’s dissertation that the student has not yet written about in a previous class – thus contributing substantively to the dissertation literature review.
...we suggest that if there is truly one "best model" for a doctor of nursing practice, it will be developed over time, in the context of the market and collegial discussion... |
In typical PhD programs students complete a dissertation seminar and then register for dissertation advisement continuously until the proposal and final dissertation is successfully defended. With our clinical dissertation, however, students are given more rigid benchmarks to mark the progress of their dissertation. After completing dissertation seminar DrNP students register for Dissertation Advisement I. They cannot register for Dissertation Advisement II until the proposal is defended and IRB materials are submitted. Next students cannot register for Dissertation Advisement III until data collection is complete. Students are then expected to spend 1-2 quarters in Dissertation Advisement III analyzing, writing, editing and then defending their clinical study. If this process has not been completed in 5 quarters (including dissertation seminar) the student will then register for Continuing Dissertation Advisement until the project is complete. Our purpose is to give the student more structure with precise benchmarks and facilitate decreasing the average 8.3 years post-MSN (versus 6.8 years for all other disciplines) it now takes a nurse to complete a doctorate (Valiga, 2004)!
Finally and perhaps most importantly, with instruction from faculty in our Department of Epidemiology and Biostatistics, our DrNP students will be grounded in the use of robust statistical procedures for small sample sizes (Hoyle, 1999), critical in the studies that will characterize our clinical dissertation design. We foresee, for example, one of our Practitioner Track students, a midwife interested in studying libido and depressive symptoms in post-partum women, first publishing her small sample size study. Subsequently, this study is then read by a nurse scientist who is intrigued by the findings and thus decides to conduct a larger clinical study, perhaps even in collaboration with this practitioner/researcher. This is the model of clinical research we want to encourage with our practice degree model.
Summary
What nursing science needs...are more nursing clinicians who will have the skills to conduct meaningful nursing research that will help expedite a greater evidence base for professional and advanced nursing practice. |
In summary, we think the critical nursing faculty shortage was a far more urgent and pressing issue for the AACN to address with such immediacy than the issue of ‘entry level preparation’ for advanced practice nurses (AACN, 2003, 2005c; Smith & Dreher, 2003). However, we suggest that if there is truly one "best model" for a doctor of nursing practice, it will be developed over time, in the context of the market and collegial discussion, as we discover what works and what doesn’t. It is unlikely to arise from a top-down imposition of rigid accreditation standards. Without the formal endorsement of any advance practice nursing organization (aside from a partial endorsement by NONPF), nor the American Nurses Association, we are already saddened to see the AACN (2005d) and the Commission on Collegiate Nursing Education (CCNE) clamping down on innovation by moving to only accredit doctor of nursing practice programs that use the ‘DNP’ initials (press release 10/20/05). But even this strategy is not likely to impede the disruptive innovators as post-master’s practice doctoral programs and clinical research practice doctoral programs will not be required to seek accreditation if they are not building licensure into their curricula.
We propose that clinical research preparation serve as the distinguishing factor...the DNP would be a professional practice doctorate and the DrNP an academic practice doctorate. |
What nursing science needs, now more than ever, are more nursing clinicians who will have the skills to conduct meaningful nursing research that will help expedite a greater evidence base for professional and advanced nursing practice. Well-designed, small scale studies can contribute greatly to our science as the number of RNs with an NIH RO1 will always be limited. To better support nursing knowledge development, the PhD needs a better practice-doctorate partner than the DNP. In the end, we believe the Drexel DrNP hybrid (as a clinical research DrNP in Nursing Science, Primary Care, Acute Care or perhaps other iterations like a DrNP in Anesthesia Science or Midwifery – all with a clinical dissertation) is an alternative practice doctorate degree for nursing faculties that do not want to entirely abandon the dissertation or the research enterprise for a new model of non-research based doctoral nursing education. We therefore propose that clinical research preparation serve as the distinguishing factor between the two practice-degree programs: the DNP would be a professional practice doctorate and the DrNP an academic practice doctorate.
We applaud the AACN for moving to mandate the doctor of nursing practice for new APNs by 2015. We only disagree with the single DNP model...[and] quest for conformity. |
We applaud the AACN for moving to mandate the doctor of nursing practice for new APNs by 2015. We only disagree with the single DNP model they selected and their quest for conformity. We contend the AACN picked the wrong health-related professional doctoral degrees to emulate as we would have sided with the more scholarly hybrids like the DrPH, PsyD, DSW, or DScPT. Nevertheless, we observe that this approaching maelstrom in nursing education will either advance our profession to levels we never imagined, or leave us to clean tons of ugly debris for decades. We can only hope that the ultimate history of the doctor of nursing practice will not parallel the ND degree. We urge more dialogue, more discussion, even prickly academic disagreement and discord among all the players and agents impacted by this decision, before we perhaps eventually settle on the doctor of nursing practice models (yes, models) that are best for nursing.
Epilogue
Our DrNP program received approval by the Pennsylvania Department of Education on April 25, 2005, so the faculty had a very limited amount of time to recruit a class that would matriculate by September 2005. In the end, the program received 21 completed applications with 14 applicants reviewed positively and given finalist interviews. Of the 14, 12 were offered admission and 11 matriculated. Their mean GRE scores were 543 verbal and 488 quantitative (total 1031). We plan to admit 15 students per year and our data base of inquiries and potential applicants now stands at 1,056. The first 11 students (5 Practitioner Track, 3 Educator Track, 2 Clinical Executive track, and 1 Clinical Scientist Track) are now finishing their first quarter of study. Six are board certified APNs and their pictures and bios can be viewed at the following web address: www.drexel.edu/cnhp/drnp_program/class-2005.asp. With our two NINR grants, one student is fully-funded and receives a stipend. We could have fully funded another student, but full-time work schedules precluded this. Six others are partially funded by a private foundation grant and several are receiving employer-supported tuition reimbursement. Two students jump-started their clinical scholarship by submitting three abstracts in only their first quarter of study, thus indicating that faculty mentoring is strong. The initial DrNP faculty was constituted by implementing a primary and secondary program appointment system within the College. Four BSN program faculty and one MSN program faculty were given a primary appointment in the DrNP program and now report to the DrNP Director. Secondary appointments were given to seven other faculty who will also teach at least one course in the program, including several nursing administrators, faculty from our School of Public Health, an RN who is a bioethicist in our Physician’s Assistant Program, and a philosopher from our Health and Society Program.
We think the reasons why this first cohort of students chose this degree model is best captured by one student interested in studying proxy decision making in the terminally ill mentally retarded adult. At his finalist interview he indicated he applied to the Drexel DrNP program because its design supported his career goals where he wanted to devote approximately 25% of his career to clinical research and knowledge development, but primarily wanted to be an expert practitioner and clinician. Finally, the Director of the DrNP program recently fielded a telephone call from a recruiter in Ohio who enthusiastically said we were preparing the precise kind of graduate the Magnet hospitals she was recruiting for were seeking – a strong clinician with a doctorate and clinical research skills. She wanted to know if we had any graduates yet?
Acknowledgements: The Doctoral Nursing Program Development Committee was instituted June 2000 by Dean Gloria F. Donnelly with Dr. H. Michael Dreher as Chair; the following individuals have served, since its inception or at some point, on this committee: Drs. Mary Ellen Smith Glasgow, Elizabeth Gonzalez, Patricia Dunphy Suplee, Kathleen Falkenstein, Albert Rundio, Kathleen Fisher, Louise Ward, Linda Wilson, Vicki Lachman, & William P. Fehder; all deserve special recognition for their contribution great or small to the development of the Drexel Model DrNP. Special thanks to Dr. Michael Dahnke for his dedicated editing assistance.
Authors
H. Michael Dreher, DNSc, RN
Email: hd26@drexel.edu
Heyward (Michael) Dreher’s primary research areas are sleep, sleep disruption with HIV disease, and sleep and aging. With a focus on sleep disorders with medical and psychiatric illness during postdoctoral study, Dr. Dreher’s current research is on sleep and depression in women living with HIV. He also maintains an interest in gerotechnology and was the PI on a recently completed three-year John A. Hartford Foundation/The American Colleges of Nursing (AACN) grant awarded to Drexel that developed the Gerontological Reasoning Informatics Project (GRIP©), a PDA-based geriatric assessment tool. He is the creator of the Circular Rank Order Technique (CROT), a new quantitative focus group technique which was refined with Dr. Smith Glasgow and recently published in the Journal of Theory Construction and Testing (2004). He has extensive experience with all levels of nursing curriculum development, and with Dr. Smith Glasgow, co-created Drexel’s 11-month BSN Accelerated Career Entry Program for second degree students (the fastest accelerated BSN degree in the country which has averaged above 98% NCLEX pass rates over the first 3 years) and the Drexel BSN-Cooperative Degree, one of only two five year nursing co-op programs in the US. He is a tenured Associate Professor and the Director of the new Doctor of Nursing Practice (DrNP) program. He was just elected to his second two-year term on the Pennsylvania State Nursing Association’s Cabinet on Clinical Practice and Professional Development and is serving in his second year as Chair. He is also currently Vice-Chair of the Drexel Faculty Senate.
Gloria F. Donnelly, PhD, RN, FAAN
Email: gd27@drexel.edu
Gloria Ferraro Donnelly serves as the Dean of the College of Nursing and Health Professions and is a tenured Full Professor. A native of Philadelphia, she is a graduate of Villanova University, the University of Pennsylvania School of Nursing, and Bryn Mawr College Department of Human Development where she completed the PhD in Human Development in 1985 as a National Service Research Pre-Doctoral Fellow.
Her interest in psychiatric-mental health nursing led her to hold clinical and educational positions at Eastern Pennsylvania Psychiatric Hospital and the Institute of the Pennsylvania Hospital in Philadelphia. She has held faculty appointments at the University of Pennsylvania School of Nursing, Trenton State College in New Jersey, and Villanova University. She was the founding Dean of Nursing at La Salle University and was the first Dean of the School of Nursing at MCP Hahnemann University which evolved into the College of Nursing and Health Professions, Drexel University. Dr. Donnelly is the author of four textbooks, and currently editor of Holistic Nursing Practice. Dr. Donnelly is a frequent contributor to the nursing education administration literature including the financial aspects of operating nursing education programs. She served as national Chair of the Council of Baccalaureate and Higher Degree Programs and a member of the Executive Committee of the Board of Governors of the National League for Nursing from 1995 to 1997. Dr. Donnelly teaches graduate nursing online courses in the College and is particularly interested in the instructional design of online courses. As one of the teaching DrNP faculty, and based on her interest in holistic nursing interventions, Dr. Donnelly will be teaching a doctoral course, ‘Self-Regulation in Health and Illness’ particularly offered for DrNP students in the Practitioner Track.
Rita C. Naremore, PhD
Email: rita.c.naremore@drexel.edu
Dr. Rita C. Naremore is Professor and Associate Dean for Research and Doctoral Education in the College of Nursing and Health Professions. She came to Drexel from Indiana University, where she served as a Department Chair for the Department of Speech and Hearing Sciences and as Associate Dean in the College of Arts and Sciences. She is an honored teacher, researcher, and editorial consultant and has served on Peer Review Committees for several federal funding agencies. Her current research activities are focused on health information technology. She recently completed a funded project with Dr. Mike Atwood in the Drexel College of Information Science and Technology investigating the use of computers equipped with Internet access and email capabilities in the management of hypertension by a group of inner city women and the nurse practitioners providing their care. In addition, she heads a team submitting an NIH proposal to demonstrate the value of handheld technology at the point of care in a nationally distributed group of women’s health clinics. Dr. Naremore also has a strong background in the scholarship of teaching and learning, particularly research investigating comprehensive methods for evaluation teaching effectiveness.
References
ACNM Division of Accreditation. (2005, June). Statement on Midwifery Education. Retrieved November 4, 2005 from the ACNM website: www.acnm.org/siteFiles/DNPstatementedited.doc
American Academy of Nurse Practitioners. (2005, October). Discussion paper: Doctor of Nursing Practice. Retrieved November 28, 2005 from the AANP website: www.aanp.org.
American Association of Colleges of Nursing (2005a). Draft AACN statement of support for clinical nurse specialists. Retrieved November 26, 2005 from the AACN website: www.aacn.nche.edu/Publications/positions/CNS11-05.htm
American Association of Colleges of Nursing (2005b). AACN applauds the National Academy of Sciences’ report which supports the practice doctorate in nursing and calls for more nurse scientists. Retrieved October 14, 2005 from the AACN website: www.aacn.nche.edu/Media/NewsReleases/2005/NASReport.htm
American Association of Colleges of Nursing. (2005c). New data confirms shortage of nursing school faculty hinders efforts to address the nation's nursing shortage. Retrieved March 18, 2005, from the AACN website: www.aacn.nche.edu/Media/NewsReleases/2005/Enrollments05.htm
American Association of Colleges of Nursing (2005d). Commission on Collegiate Nursing Education moves to consider for accreditation only practice doctorates with the DNP degree title. Retrieved October 24, 2005 from the AACN website: www.aacn.nche.edu/Media/NewsReleases/2005/CCNEDNP.htm
American Association of Colleges of Nursing. (2004a). AACN position statement on the practice doctorate in nursing. Retrieved June 8, 2005 from the AACN website: www.aacn.nche.edu/DNP/pdf/DNP.pdf
American Association of Colleges of Nursing. (2004b). 2004 annual state of the schools. Washington, DC: Author.
American Association of Colleges of Nursing. (2003). White paper: Faculty shortages in baccalaureate and graduate nursing programs: Scope of the problem and strategies for expanding the supply. Washington, DC: Author.
American Association of Nurse Anesthetists. (2005, June). Report of the American Association of Nurse Anesthetist’s Summit on Doctoral Preparation for Nurse Anesthetists. Retrieved November 4, 2005 from the AANA website: http://www.aana.com/uploadedFiles/Professional_Development/Nurse_Anesthesia_Education/Educational_Resources/DNP/DNP%20Summit%20Final%20Report.pdf
American Dental Association. (2005, March 14). American Dental Association: Dental definitions. Retrieved November 24, 2005 from dentistry.about.com website: http://dentistry.about.com.
Boston University Sargent College of Health and Rehabilitation Science (2004). Programs: Audiology, Doctor of Science. Retrieved June 8, 2005 from the Boston University website: www.bu.edu/sargent/programs/graduate/audiology/research_track.html
Christensen, C. M., & Raynor, M. E. (2003). The innovators solution: Creating and sustaining successful growth. Boston, MA: Harvard Business School Press.
Council on Accreditation of Nurse Anesthesia Educational Programs. (2003). Trial standards for accreditation of nurse anesthesia programs. Park Ridge, IL: Author.
Council on Accreditation of Nurse Anesthesia Educational Programs. (2004). Standards for accreditation of nurse anesthesia programs. Park Ridge, IL: Author.
Dreher, H.M., Smith Glasgow, M.E., Gonzalez, E., Suplee, P., Falkenstein, K., & Rundio, A. (2005). Drexel University College of Nursing and Health Professions Doctor of Nursing Practice: Proposal submitted to the Commonwealth of Pennsylvania for DrNP in Nursing Science degree approval. Unpublished manuscript.
Fitzpatrick, J. (2003). The case for the clinical doctorate in nursing. Reflections on Nursing Leadership, 8, 37.
Gennaro, S. (2004). A rose by any other name? Journal of Professional Nursing, 20, 277-278.
Hoyle, R. (1999). Statistical strategies for small sample research. Thousand Oaks, CA: Sage Publications.
Kinslow, K. (2005, September). Practice doctorate in nursing: American Association of Nurse Anesthetist’s perspective. Paper presented at the Pennsylvania State Nurses Association Pre-conference Session on ‘The Dilemma over the Doctor of Nursing Practice (DNP): Different Perspectives,’ Harrisburg, PA.
Lee, J.M., Furner, S., Yager, J., & Hoffman, D. (2003, June). A review of the status of the doctor of public health (Dr.P.H.) degree. Paper presented at the American Public Health Association (ASPH) Associate Dean’s Retreat, Grouse Mountain Lodge, Whitefish, MT.
Murray, B. (2000, January). The degree that almost wasn’t: The PsyD comes of age. Monitor on Psychology, 31, 1-5. Retrieved April 4, 2005 from www.apa.org/monitor/jan00/ed1.html
National Academy of Sciences. (2005). Advancing the nation’s health needs. Committee for monitoring the nation’s changing needs for biomedical, behavioral, and clinical personnel. Washington, DC: The National Academies Press.
National Association of Clinical Nurse Specialists. (2005a, April). White paper on the Nursing Practice Doctorate. Retrieved May 20, 2005 from the NACNS website: http://www.nacns.org/LinkClick.aspx?fileticket=xHLMMgMYJ98%3d&tabid=116
National Association of Clinical Nurse Specialists. (2005b, September). NACNS update on the clinical nurse leader (CNL) September 2005. Retrieved November 26, 2005 from the NACNS website: http://www.nacns.org/LinkClick.aspx?fileticket=3%2bip4nbDLho%3d&tabid=116
O’Sullivan, A. L. (2005). The practice doctorate in nursing. The Mentor, 16, 2-3, 12.
Peterson, D.R. (1976). Need for the doctor of psychology degree in professional psychology. American Psychologist, 31, 792-798.
Peterson, D.R. (1982). Origins and development of the doctor of psychology concept. In G.R. Caddy, D.C. Rimm, N. Watson, & J.H. Johnson (Eds.), Educating professional psychologists (pp. 19-38). New Brunswick, NJ: Transaction Books.
Rutgers University. (2005). Rutgers University New Brunswick/Piscataway campus: The Graduate School of Applied and Professional Psychology dissertations. Retrieved November 25, 2005 from the Rutgers website: http://gsappweb.rutgers.edu/cstudents/dissertations/dissertation%20titles.php.
Smith, M.E., & Dreher, H.M. (2003).Wanted, nursing faculty! If you think the nursing shortage is bad, the nursing faculty shortage is worse. Advances for Nursing, 5, 31-32.
Stein-Parbury, J. (2000, May). Nursing around the world: Australia. Online Journal of Issues in Nursing [On-line serial]. 5(2), Manuscript 3. Available www.nursingworld.org/MainMenuCategories/OJIN/TableofContents/Volume52000/No2May00/NursinginAustralia.aspx
University of Alabama at Birmingham Department of Physical Therapy, School of Health Related Professions. (2005). Doctor of Science in Physical Therapy. Retrieved June 8, 2005 from UAB website: http://main.uab.edu/shrp/default.aspx?pid=80258
University of Queensland, Brisbane, Australia. (2004). Professional doctorate program. Retrieved March 20, 2005 from University of Queensland website: www.uq.edu.au/international/?page=978&pid=978&ntemplate=415
Valiga, T. (2004). The nursing faculty shortage: A national perspective. Congressional briefing presented by the A.N.S.R. Alliance, Hart Senate Office Building, Washington, DC.
Wheaton College. (2004). Clinical dissertation manual for the doctor of psychology degree (Psy.D). Wheaton College Psychology Department. Wheaton, IL: Author.
Widener University. (2004). Manual for the clinical dissertation for the doctor of psychology degree (PsyD). Widener University Institute of Graduate Clinical Psychology. Chester, PA: Author.

